WHAT IS BLOOD CANCER?
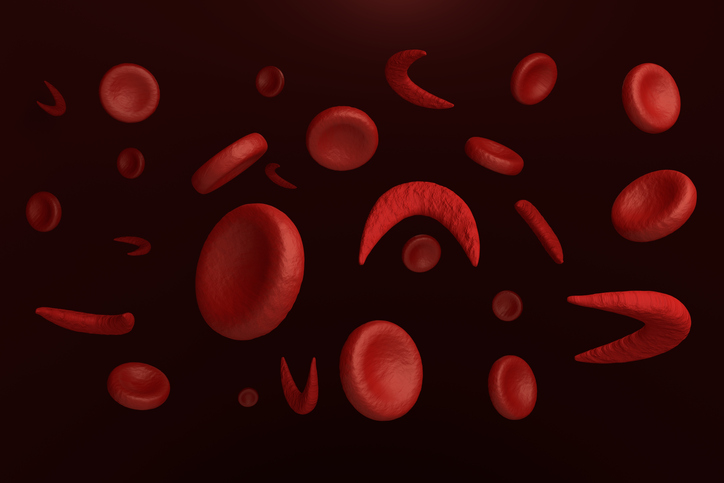
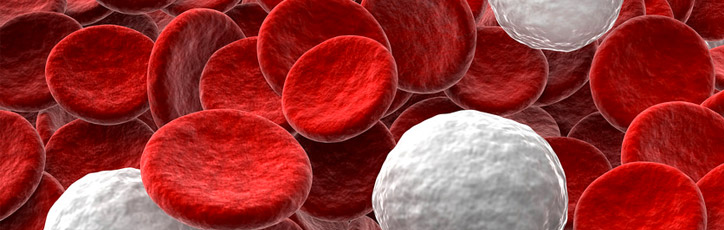
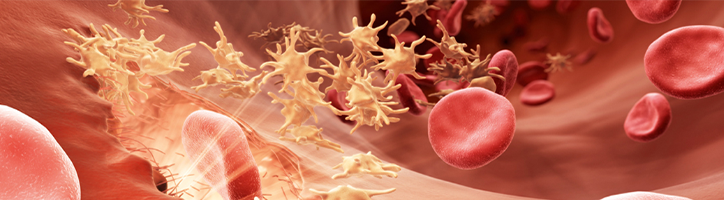
Your blood is made up of different cell types including red blood cells for carrying oxygen, platelets to help blood clot and white blood cells that fight infections. They all originally come from stem cells, which have the potential to develop into any type of blood cell as they divide and mature. Problems in this process, known as ‘differentiation’, are at the root of all blood cancers. Different types of blood cancer depend on when and how these problems occur.
These problems often lead to your body producing large numbers of immature blood cells that can’t perform their job properly. They can also ‘clog up’ your bone marrow, which prevents other types of blood cells from doing their job too.
Unfortunately, blood cancer affects a large number of people. Every 40 seconds, someone in India is told they have blood cancer. That’s 2160 people a day. So you are certainly not alone.
Blood cancers are categorised into three groups. We have gathered information on some of the more common examples of each group so you can learn more about your circumstance. We also link to organisations that offer additional advice and support.
The what are my treatment options? section looks at other possible ways that your medical team might decide to treat your cancer - either before or instead of a stem cell transplant.

Leukaemia
Leukaemias are cancers that affect your blood cells, mainly your white blood cells and bone marrow. These cells often divide too quickly and don’t develop properly, which compromises your immune system and ability to fight infections.
Many types of leukaemia are either ‘acute’ or ‘chronic’ based on how they behave. In general, acute conditions develop very quickly and need treating aggressively straight away. Chronic conditions usually progress more slowly and intensive treatment may not be needed straight away.
There are four main types of leukaemia:
- Acute myeloid leukaemia (AML)
- Acute lymphoblastic leukaemia (ALL)
- Chronic myeloid leukaemia (CML)
- Chronic lymphocytic leukaemia (CLL)
Other types of leukaemia include:
- acute promyelocytic leukaemia (APL)
- hairy cell leukaemia (HCL)
- large granular lymphocytic leukaemia (LGL)
- t-cell acute lymphoblastic leukaemia (T-ALL)
- chronic myelomonocytic leukaemia (CMML)
If you would like more information on less common types of leukaemia or myeloproliferative neoplasms that are related to leukaemia, you can visit Leukaemia Care, Bloodwise or Cancer Research UK.
Lymphoma
Lymphoma is a type of blood cancer that affects your lymphatic system, an important part of your immune system that produces and transports white blood cells around your body. It also removes waste products from your blood.
Lymphoma can develop in many parts of your body, including your lymph nodes, bone marrow, blood, spleen and other organs.
There are two main types of lymphoma, based on how they behave and their treatment:
More detailed information about less common types of lymphoma can be found on the Lymphoma Association website.
Myeloma
Myeloma (also referred to as multiple myeloma) is a blood cancer that affects a certain type of white blood cell called a plasma cell. These cells are made in your bone marrow and produce antibodies which help fight infection.
Our Myeloma page has more information.
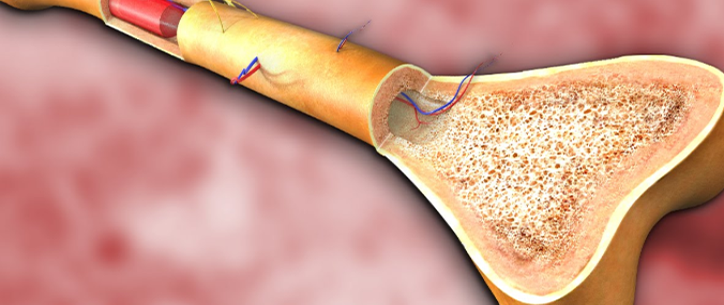
BONE MARROW AND TRANSPLANTATION
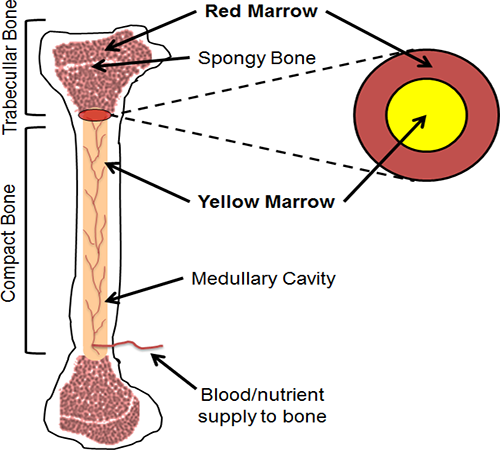
Bone marrow is the soft, spongy center of your bone where blood is produced. Most people who need to undergo a bone marrow transplant have cancer, such as leukemia or lymphoma. There are different types of bone marrow transplants. The type and severity of your disease determine what type of transplant you will need.
Blood & Marrow Transplant Program
The mission of the Blood & Marrow Transplant (BMT) Program in the Taussig Cancer Institute is to provide high quality specialized patient care in a setting of education and research.
How the bone marrow functions
Bone marrow is the soft, spongy center of your bone where blood is produced. Marrow is filled with blood-producing cells, called hematopoietic progenitor cells (HPCs), which develop into mature white blood cells, red blood cells, or platelets.
- White blood cells of various kinds make up part of your immune system for fighting infections.
- Red blood cells are responsible for carrying oxygen throughout your body.
- Platelets clot your blood to prevent bleeding.
HPCs are constantly being produced by your bone marrow, and will develop into the types of cells your body needs. HPCs are sometimes called stem cells.
Types of bone marrow transplants
Most people who need to undergo a blood or marrow transplant have cancer, such as leukemia, lymphoma or multiple myeloma. There are different types of transplants. The type and severity of your disease determine what type of transplant you will need.
An allogeneic transplant involves receiving donor bone marrow, umbilical cord stem cells, or peripheral stem cells. This donor is genetically matched and can be related or unrelated to you.
An autologous transplant involves receiving your own bone marrow or peripheral blood stem cells. A syngeneic transplant involves receiving your identical twin's bone marrow or peripheral stem cells. Here is more information about the specific types of blood or marrow transplants:
An allogeneic transplant involves receiving very high-doses of chemotherapy and/or radiation therapy, followed by the infusion of your donor's bone marrow or peripheral blood stem cells. The high-dose cancer-fighting treatments are given to eliminate the cancer in your body.
The infusion of the new marrow, cord blood, or peripheral stem cells from the donor replaces the bone marrow destroyed by the chemotherapy and/or radiation therapy. Allogeneic transplant patients have the risk of developing a complication called graft-versus-host disease or GvHD. GvHD is a condition where donor cells from the graft attack the patient's (or host's) organs or tissues The condition can be mild and treated on an outpatient basis, or it can be severe and require treatment in the hospital.
You might be a potential candidate for an allogeneic transplant if you have leukemia, aplastic anemia, myelodysplasia, myelofibrosis, high-grade lymphoma or other types of cancers.
A reduced intensity allogeneic transplant involves receiving lower doses of chemotherapy and radiation therapy followed by the infusion of your donor's bone marrow or peripheral blood stem cells. The objective is to suppress your own bone marrow by receiving just enough chemotherapy and radiation therapy to allow your donor cells to engraft and grow within you. The hope is these donor cells will mount an immunologic attack against your underlying cancer, generating a response called the “graft-versus-leukemia” effect or “graft-versus-cancer” effect.
You might be a potential candidate for this type of transplant if you have a slow-growing, indolent disorder, such as chronic leukemia, multiple myeloma, myelodysplasia, and low-grade lymphoma.
The mini allogeneic transplant is not appropriate, for example, if you have fast- growing acute leukemia.
An autologous bone marrow transplant involves receiving very high-dose chemotherapy followed by the infusion of your previously collected peripheral stem cells or bone marrow.
The high-dose chemotherapy treatments are given to eliminate the cancer in your body. The infusion of your new marrow or peripheral stem cells replaces the bone marrow destroyed by the chemotherapy and/or radiation therapy.
You might be a potential candidate for an autologous transplant if you have lymphoma, multiple myeloma, Hodgkin's disease, germ cell cancer, or certain types of leukemia.
Pre-transplant evaluation
Before a blood or marrow transplant can be approved as a treatment option, you will have a pre-transplant evaluation. This evaluation includes a complete physical, consultations with members of the Transplant Team, and a comprehensive series of tests. A pre-transplant evaluation provides complete information about your overall health and helps determine if you are eligible for a blood or marrow transplant.
Blood or marrow transplantation as a treatment option
After your transplant doctor has determined you are a good candidate for a transplant, a date for the transplant will be determined and the process of insurance clearance will begin. Please understand that insurance reimbursement for transplantation is not automatic.
If you are to be admitted to the hospital for your transplant, you can expect your stay to be about 3 to 4 weeks, depending on your recovery. During your recovery, you will learn about your new medicines, how to recognize signs of complications and infections, and when you can return to your normal activities.
If an outpatient reduced intensity allogeneic transplant has been approved for you, you will be required to stay within a one-hour drive of Cleveland Clinic’s main campus for at least 100 days after your transplant. At that time, your doctor will evaluate your medical condition to determine where you can continue your follow-up care.
TYPES OF BLOOD DISORDER IN CHILDERNS AND TEENS
There are many types of blood disorders, which can involve problems with red blood cells, white blood cells, platelets, blood vessels, bone marrow, lymph nodes, or the proteins involved in bleeding and clotting.
At our Blood Disorders Center, patients receive care from some of the world’s most experienced pediatric hematologists with deep experience in the conditions we treat, including:
Red blood cell and iron disorders
- Red blood cell disorders overview
- Anemia overview
- Sickle cell disease
- Thalassemia
- Hemolytic disease of the newborn
- Hemolytic anemia
- Spherocytosis
- Iron deficiency anemia
- Hemochromatosis
- Iron-refractory iron deficiency anemia (IRIDA)
- Congenital sideroblastic anemia
- Congenital dyserythropoietic anemia
- Megaloblastic anemia (including pernicious anemia)
White blood cell disorders
- White blood cell disorders overview
- Severe congenital neutropenia (Kostmann syndrome)
- Cyclical neutropenia
- Chronic granulomatous disease
- Leukocyte adhesion deficiency
- Myeloperoxidase deficiency
Bone marrow failure syndromes
- Aplastic anemia
- Congenital amegakaryocytic thrombocytopenia
- Diamond-Blackfan anemia
- Dyskeratosis congenita
- Fanconi anemia
- Myelodysplastic syndrome (MDS)
- Schwachman-Diamond syndrome
- Thrombocytopenia absent radius
Bleeding disorders
- Hemophilia
- von Willebrand disease
- Platelet function disorders
- Thrombocytopenia
- Hypofibrinogenemia and dysfibrinogenemia
Autoimmune blood cell disorders